When it comes to Pregnancy, understanding Microchimerism is vital for practitioners and mothers to be.
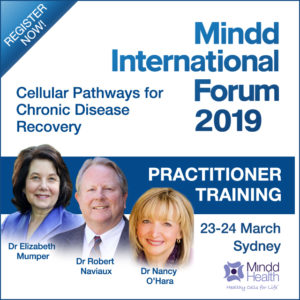
Mindd International Forum, 23-24 March (Live in Sydney, Australia and Livestreaming globally)
Certified practitioners who pass the assessment will be listed at mindd.org. A certificate of completion will be provided for CPD applications.
Leah Hechtman will be a guest speaker at the 2019 Mindd Forum. She is the director of The Natural Health and Fertility Centre in Sydney and has been in practice for over 20 years. She specialises in fertility, pregnancy and reproductive healthcare for men and women. Leah has completed extensive advanced training and is currently completing her PhD through the School of Women’s and Children’s Health (Faculty of Medicine [UNSW]).
Leah will be speaking on the topics of Microchimerism, mRNA and Parental Wisdom, which is the understanding of how pregnancy can change the health of a mother in unintended ways. Leah’s expertise extends to how we can influence unique genetic pathways to improve the health of future generations. She will be discussing the latest research regarding these fascinating areas at the Forum and how practitioners can apply this knowledge in clinical practice.
What is Microchimerism?
Microchimerism refers to cells, or DNA, derived from an individual that originated in a genetically separate environment. This can be due to the transfer of cells between a mother and fetus. Research shows that miscarriage or an induced abortion can also produce this condition, as well as being pregnant to twins as a transfer of cells can take place between the fetuses. Research is currently evaluating the likelihood of whether an older sibling/previous pregnancy can pass cells to a current fetus of a different pregnancy.
When present, the immune response to the exchange of these fetal cells changes the basic physiology of the mother. The cells are left behind in the mother and can either be harmful or helpful depending on many variables. Maternal microchimerism can persist into adult life for the offspring in immune competent and healthy individuals, and mothers have microchimerism of fetal origin many years after childbirth.
How is Microchimerism Detected?
It is usually detected by DNA and cellular testing. DNA is extracted from peripheral blood or tissues and evaluated for genetic polymorphisms that are absent in the test subject. “The most common DNA-based approach is testing for male DNA in a female as a marker for presumed prior pregnancy with a male fetus” (Nelson, 2012).
Are There Health Problems Associated with Microchimerism?
The question as to whether microchimerism and genetically different cells can affect long-term health is a valid one since the cells can persist. The condition has been identified in multiple tissues in humans and not just in disease states. Normal, healthy tissue can have these foreign cells present. Research is currently assessing whether microchimerism has a positive, neutral or negative effect on the host. Since there are many variables, it is not a straightforward conclusion. Things such as the origin of the cells, how they were acquired, the type of cells, the duration of time since the acquisition of the cells and the age of the host are all variable factors affecting the outcome of this conclusion.
Potential Benefits Associated with Microchimerism
While the main focus area of microchimerism has been centred on its potential to cause harm, there is also a more positive outlook beginning to surface. It has been hypothesised that microchimerism fetal cells may have the ability to provide repair processes within maternal tissue. This was originally seen in the capability of mammals to save their mother’s lives by providing cells that were repairing tissue, including bone marrow, to replace dysfunctional cells.
Current Research
The key area research is currently focusing on is microchimerism and autoimmune disease. It is presently known that microchimerism can be found in the immune cells of offspring, specifically in the T and B cells, natural killer cells and macrophages. Microchimerism of fetal origin is also showing that it has the potential to differentiate into specific cell types found within the tissue. Male cells were detected in the thyroid, intestine, gallbladder and cervix in women, as well as expressing a hepatocyte marker in women with multiple conditions, some of which are autoimmune.
Systemic sclerosis (SSc) which is an autoimmune disease has an increased incidence in women in post-reproductive years. Studies have identified microchimerism of both fetal and maternal origin in blood and tissues of patients with this condition. The characteristics and interactions of microchimeric cells in SSc tissues is not well understood, and the pathogenesis is presently unclear and unknown. “One hypothesis is that microchimeric antigens are presented by patient antigen-presenting cells to patient T cells, referred to as the indirect pathway, a mechanism thought to underlie chronic organ rejection” (Nelson, 2012).
Epidemiological and immunogenetic studies in rheumatoid arthritis and microchimerism also depict the potential for beneficial as well as adverse consequences of maternal and fetal origin microchimerism. Much more research is needed in this area before it can be determined as a contributing factor.
Learn more about this fascinating topic and its potential to affect future generations at Leah Hechtman’s Presentation on Microchimerism
For more information on the Forum or to register (Live or Livestream) visit the Speakers and Program page…
Reference list: